Practice Policies & Patient Information
CCTV Policy
Introduction and Objectives
A Closed-Circuit Television System (CCTV) has been introduced by Arcadian Gardens Surgery (“the Practice”) comprising a number of cameras that are fixed. All cameras are fully operational.
The owner of the system is the Practice.
For the purposes of the UK Data Protection Legislation, the data controller is the Practice, which is registered with the Information Commissioner, registration ZA327350.
The system manager is the GP Principal, DR M C K PERERA. The GP Principal is also the key contact point, and should be contacted via the Practice’s normal contact details on the website for any issues relating to the system
It is recognised that operation of the Practice’s CCTV System may be considered to infringe on the privacy of individuals. The Practice recognises that it is their responsibility to ensure that CCTV on the premises should always comply with all relevant legislation, to ensure its legality and legitimacy. CCTV will only be used as a proportional response to identified problems and be used only in so far as it is necessary in a democratic society, in the interests of national security, public safety, the economic well-being of the area, for the prevention and detection of crime or disorder, for the protection of health and morals, or for the protection of the rights and freedoms of others.
The legislation concerning CCTV in Section 30 of the Protection of Freedoms Act 2012 has produced a CCTV Code of Practice from the Surveillance Camera Commissioner that has been approved by Parliament and the Practice must pay due regard to the code.
The Practice in managing its CCTV operations under this Code of practice will endorse and comply with all 12 guiding principles of the Surveillance Camera Code of Practice.
The Codes of Practice and observance of the Operational Procedures contained in the policy shall ensure that evidence is secured, retained and made available as required to ensure there is absolute respect for everyone’s right to a free trial.The Practice CCTV System shall be operated with respect for all individuals, recognising the right to be free from inhuman or degrading treatment and avoiding discrimination on any ground such as sex, race, colour, language, religion, political or other opinion, national or social origin, association with a national minority, property, birth or other status.
Objectives
The objectives of the Practice CCTV System which form the lawful basis for the processing of data are: –
• To help deter crime and reduce the fear of crime
• To ensure the safety of persons in or near our premises and vehicles
• To protect our property from theft, vandalism and other threats
• To help detect crime and disorder, or other public safety issues
• To provide evidential material suitable for court proceedings, dispute resolution and civil proceedings
• To assist in supporting civil proceedings
• To assist in the overall management of the Practice, including dispute resolution and discipline management
Procedures
The GP Principal will provide access to the system where this is required. In their absence, the Practice Manager or Senior Partner will provide access.
Recordings will only be accessed where an incident has occurred or is suspected which falls within the objectives above. Review of recordings will take place only under supervision, and export of recordings will only be permitted where there is a legal requirement to do so. The persons involved in an incident may be present to review the information (including patients) where this is deemed necessary.
A record will be made of all uses of recordings and who viewed them.
Recording will be redacted (identifiable information such as faces blurred) when requested as part of a Subject Access Request.
How we comply with the code
Principle 1 Use of a surveillance camera system must always be for a specified purpose which is in pursuit of a legitimate aim and necessary to meet an identified pressing need.The specific purposes are given in Objectives above. There is a pressing need for the Practice to ensure the safety of its staff, patients and visitors, and to protect its assets.
Principle 2 The user of a surveillance camera system must take into account its effect on individuals and their privacy, with regular reviews to ensure its use remains justified.
This has been carefully considered. Fixed cameras record continuously within their scope and public areas are excluded from scope. Mobile cameras are not used.
Cameras are not placed in enclosed areas where there is an expectation of privacy e.g. bathrooms/toilets etc.
Principle 3 There must be as much transparency in the use of a surveillance camera system as possible, including a published contact point for access to information and complaints.
This is provided by this policy.
Principle 4 There must be clear responsibility and accountability for all surveillance camera system activities including images and information collected, held and used.
The Operations Manager/Practice manager is responsible and accountable for all activities
Principle 5 Clear rules, policies and procedures must be in place before a surveillance camera system is used, and these must be communicated to all who need to comply with them.
These are provided by this policy
Principle 6 No more images and information should be stored than that which is strictly required for the stated purpose of a surveillance camera system, and such images and information should be deleted once their purposes have been discharged.
Recordings made by detection are deleted after 30 days unless action is taken to preserve them. This is only done where the recordings are required for one of the objectives noted above.
Principle 7 Access to retained images and information should be restricted and there must be clearly defined rules on who can gain access and for what purpose such access is granted; the disclosure of images and information should only take place when it is necessary for such a purpose or for law enforcement purposes.
Only the roles noted above can access images except where required by law enforcement. The roles noted above will manage the viewing of images in normaluse to meet the objectives above. Viewing of images by persons involved in incidents will be granted where necessary for the objectives.
Principle 8 Surveillance camera system operators should consider any approved operational, technical and competency standards relevant to a system and its purpose and work to meet and maintain those standards.
These have been considered. As a technical standard, we have a minimum image size of 1080p to ensure sufficient clarity. However the resolution is not sufficient to allow document or computer screens to be read from the CCTV system.
Principle 9 Surveillance camera system images and information should be subject to appropriate security measures to safeguard against unauthorised access and use.
Images are stored on the servers at the Practice. These are appropriately secured.
Principle 10 There should be effective review and audit mechanisms to ensure legal requirements, policies and standards are complied with in practice, and regular reports should be published.
This policy is reviewed annually, the review date is at the end. No reporting is considered necessary by the practice except for logging of details of individual accesses for the purposes.
Principle 11 When the use of a surveillance camera system is in pursuit of a legitimate aim, and there is a pressing need for its use, it should then be used in the most effective way to support public safety and law enforcement with the aim of processing images and information of evidential value.
This principle is supported by this document.
Principle 12 Any information used to support a surveillance camera system which compares against a reference database for matching purposes should be accurate and kept up to date.
No reference databases are used.
Last updated June 2023.
Code of Behaviour for Patients and Visitors
Complaints Form and Policy
Submit a complaint using our online form.
Print off complaints form and the following complaints policy.
Important Notice
If you have a complaint or concern about the service you have received from the doctors or any of the staff working in this practice, please let us know by completing the form on this page.
We operate a practice complaint procedure as part of an NHS complaints system, which meets or exceeds national criteria. We hope that we can sort most problems out easily and quickly, often at the time they arise and with the person concerned. We make every effort to give the best service possible to everyone who attends our Practice.
However, we are aware that things can go wrong, resulting in a patient feeling that they have a genuine cause for complaint. If this is so, we would like the matter to be settled as quickly, and as amicably, as possible.
To have your complaint investigated, you need to complain within 12 months of the event happening, or as soon as you first become aware of the issue you want to complain about.
The time limit can be extended in special circumstances.
Interpreting Service
We can arrange for a meeting with the Practice Manager and an Interpreter for any patient whose first language is not English and needs help with their complaint.
How to make a compliment or complaint
Whether you are happy or unhappy with the care and treatment that you have received, please get in touch and let us know your views.
Receiving compliments and complaints is important to ensuring good quality local healthcare in our Practice – helping us to find out more about what we’re getting right and what we can improve.
We hope this will help you to make your feelings and experiences known to the appropriate people. Should you have a complaint we hope this page will give you more information about what to do, who to contact and what happens next.
How do I raise a concern / informal complaint?
You can speak to any member of staff initially with your complaint. This gives you the opportunity to resolve any concern you may have without it going through a formal process.
Most complaints are best resolved within the practice and these should be made via the Practice Manager.
Formal Complaint
What we will do
We will contact you about your complaint within three working days and offer to discuss with you the best way to investigate it, including the time scales for a reply. We will aim to offer you an explanation within that time frame. Or a meeting with the people involved.
-
- Find out what happened and what went wrong
- Invite you to discuss the problem with those involved, if you would like this
- Apologise where this is appropriate
- Identify what we can do to make sure that the problem does not happen again.
If you feel you do not want to contact the surgery directly, then you can contact the NHS Complaints team on:
NHS England, PO Box 16738, Redditch, B97 9PT
If you are making a complaint please state: ‘For the attention of the complaints team’ in the subject line. Contact information for NHS England can be found here.
In General
If you have a complaint to make, you can either contact the Practice Manager or ask the Receptionist for a copy of our Complaints Procedure. We will endeavour to:
-
- acknowledge any letter or Complaints Form within 3 working days of receiving it.
- deal with the matter as promptly as possible – usually within 20 working days – dependent on the nature of the complaint.
Who can complain
Complainants may be current or former patients, or their nominated or elected representatives (who have been given consent to act on the patients behalf).
-
- Patients over the age of 16 whose mental capacity is unimpaired should normally complain themselves or authorise someone to bring a complaint on their behalf.
- Children under the age of 16 can also make their own complaint, if they’re able to do so.
If a patient lacks capacity to make decisions, their representative must be able to demonstrate sufficient interest in the patient’s welfare and be an appropriate person to act on their behalf. This could be a partner, relative or someone appointed under the Mental Capacity Act 2005 with lasting power of attorney.
Appropriate person
In certain circumstances, we need to check that a representative is the appropriate person to make a complaint.
-
- For example, if the complaint involves a child, we must satisfy ourselves that there are reasonable grounds for the representative to complain, rather than the child concerned.
- If the patient is a child or a patient who lacks capacity, we must also be satisfied that the representative is acting in the patient’s best interests.
If we are not satisfied that the representative is an appropriate person we will not consider the complaint, and will give the representative the reasons for our decision in writing.
Time limits
A complaint must be made within 12 months, either from the date of the incident or from when the complainant first knew about it.
The regulations state that a responsible body should only consider a complaint after this time limit if:
-
- the complainant has good reason for doing so, and
- it’s still possible to investigate the complaint fairly and effectively, despite the delay.
Procedure
We have a two stage complaints procedure. We will always try to deal with your complaint quickly however if it is clear that the matter will need a detailed investigation, we will notify you and then keep you updated on our progress.
Stage one – Early, local resolution
We will try to resolve your complaint within five working days if possible.
If you are dissatisfied with our response, you can ask us to escalate your complaint to Stage Two.
Stage Two – Investigation
-
- We will look at your complaint at this stage if you are dissatisfied with our response at Stage One.
- We also escalate some complaints straight to this stage, if it is clear that they are complex or need detailed investigation.
- We will acknowledge your complaint within 3 working days and we will give you our decision as soon as possible. This will be no more that 20 working days unless there is clearly a good reason for needing more time to respond.
Complain to the Ombudsman
If, after receiving our final decision, you remain dissatisfied you may take your complaint to the Ombudsman.
The Ombudsman is independent of the NHS and free to use. It can help resolve your complaint, and tell the NHS how to put things right if it has got them wrong.
The Ombudsman only has legal powers to investigate certain complaints. You must have received a final response from the Practice before the Ombudsman can look at your complaint and it will generally not look into your complaint if it happened more than 12 months ago, unless there are exceptional circumstances.
Address:
Parliamentary & Health Service Ombudsman, Tower 30, Millbank, London, SW1P 4QP
Phone: 0345 015 4033
More information to the Ombudsman
Independent Complaints Advocacy Service (ICAS)
If you have concerns about or wish to make a complaint about the quality of care you receive from the NHS, or any other issues or experiences when using the NHS, ICAS can help. People using the health service usually feel they can raise such concerns with a member of staff, such as a Therapist, Doctor, Nurse or Receptionist and the NHS expects that the person you approach will do their best to help you. However, if you are not satisfied by their response or prefer to talk to someone who is not directly involved in your healthcare, ICAS is there to help.
ICAS provide a service which aims to improve your satisfaction and reduce any confusion or anxiety you may have and ICAS staff will act as quickly, and creatively, as possible to support patients, their carers and families to deal with concerns before they become more serious.
Complaints resolution staff at your Practice should give you further information about making a complaint and assist you in contacting ICAS, should you require help with your complaint from outside the NHS.
Please refer to the ICAS website for more information.
Telephone: 0300 330 5454
Confidentiality
All complaints will be treated in the strictest confidence.
Where the investigation of the complaint requires consideration of the patient’s medical records, we will inform the patient or person acting on his/her behalf if the investigation will involve disclosure of information contained in those records to a person other than the Practice or an employee of the Practice.
We keep a record of all complaints and copies of all correspondence relating to complaints, but such records will be kept separate from patients’ medical records.
Statistics and reporting
The Practice must submit to the local primary care organisation periodically/at agreed intervals details of the number of complaints received and actioned.
There Are A Number Of Sources Who Can Help You Make Your Decisions And Give Advice:
These include:
The Citizens Advice Bureau
Find your local Citizens Advice – Citizens Advice
NHS Complaints Independent Advocacy Service,
Tel: 0300 330 5454 or email via their web-site.
(Includes VoiceAbility)
POhWER (An advocacy service that also provides advocacy under the Care Act)
Tel: 03000 456 2370 or email via their web-site.
Heathwatch Haringey (can direct you to other advocacy services)
Tottenham Town Hall, Town Hall Approach Road, London, N15 4RX
Tel: 020 8888 0579
Did not attend
Missing two or more appointments within a year can lead to you receiving a letter from the practice. You’ll get warnings and a chance to explain the reason why you could not attend, but persistent no-shows will result in removal from the patient list of the surgery and you having to find a new doctor.
Dignity and Respect
How we use your health and care data to improve care

For more information or if you don’t want your data shared please click here or scan the QR code. 
You can also call 020 3198 8738 or email nclicb.digitalhelpdesk@nhs.net
Infection Prevention and Control
To view our full Infection Prevention and Control Audit Report and Action Plan, click here.
NHS Information Sharing
Click here for more information about sharing information from your health records
NHS Treatment when travelling abroad
Under NHS legislation, the NHS ceases to have responsibility for people when they leave the UK to live abroad on a permanent basis. This is because the NHS is a Residency Based System.
People traveling within Europe should be advised to carry either a UK Global Health Insurance Card (UK GHIC) (for most people) or a UK European Health Insurance Card (UK EHIC) if you have rights under the Withdrawal Agreement which entitles them to medically necessary state-provided healthcare whilst in a European Union (EU) country or Switzerland.. Not all state healthcare is free within the EU and Switzerland and so you may have to pay for services that you would get for free on the NHS. For most people, the UK Global Health Insurance Card (UK GHIC) replaces the existing European Health Insurance Card (EHIC) for new applications.
Requests for extra supplies of medications for patients who wish to travel abroad
The BMA guidance on prescribing in General Practice states that the NHS accepts responsibility for supplying ongoing medication for temporary periods abroad of up to three months. This applies for both holidays and working abroad. If a person is going to be abroad for more than three months, then only a sufficient supply of his/her regular medication should be provided to enable them to get to the destination and find an alternative supply. The patient should be advised to register with a local doctor for continuing medication, which they may need to pay for; the patient should check if the medicines required are available in the country being visited. GP practices however are not responsible for finding a doctor or ensuring medication supplies are available at the holiday destination. The patient is responsible for finding and registering with a local doctor and for confirming a regular supply of their medication. NHS prescriptions must never be obtained by relatives or friends on behalf of patients who are currently abroad, irrespective of such factors as owning a house in the UK or paying UK taxes. Patients are responsible for ensuring that any drugs they take into a country conform to local laws Further information is available on the NHS website and the UK government website.
Controlled drugs and travellers
A personal import/export licence is not required by the Home Office if a person travelling abroad is carrying less than3 months’ supply of a controlled drug (schedules 2, 3, or 4 Part I (CD Benz) and Part II (CD Anab), but is required for longer periods. See the BNF. Advice to prescriber – It is advised that a covering letter from the prescriber is obtained that confirms the name of the patient, travel plans, the name of the prescribed controlled drug, total quantity and dose. Patient responsibilities – The patient should check with the embassies or High Commission for the countries they will be travelling through to ensure that import and export regulations in those countries are complied with Patients should also check any additional requirements that their travel operator/airline company may impose. Patients can obtain further information on carrying controlled drugs abroad from Bringing medicine containing a controlled drug into the UK.
Planning your healthcare abroad
If you’re moving abroad on a permanent basis, you’ll no longer automatically be entitled to medical treatment under normal NHS rules. This is because the NHS is a residence-based healthcare system.
You’ll have to notify your GP practice so you and your family can be removed from the NHS register.
Before leaving for your new destination, it’s important to check what health services are available to you in that country.
Healthcare systems vary from country to country and might not include services you’d expect to get free of charge on the NHS. You may have to pay a patient contribution towards any treatment you get, or it may be necessary to take out health insurance.
The Foreign, Commonwealth and Development Office (FCDO) provides useful information for British nationals living abroad on GOV.UK, including information on entry and residence requirements, health, benefits and finance.
Information:
Find out how UK nationals can access healthcare in the EU, Norway, Iceland, Liechtenstein and Switzerland on GOV.UK
In most countries, you’ll have to register with the relevant authorities.
Once you’re registered as a resident, to work and make social security (national insurance) contributions, you’ll be entitled to state-run healthcare on the same basis as a resident of that country. Even if you’re not working, many countries expect you to make patient contributions or to join a national health insurance scheme.
Moving to Europe
There are circumstances in which you might be entitled to healthcare paid for by the UK.
This will depend on whether you want to live abroad permanently or only work outside the UK for a set period. The assistance available only applies within the European Union (EU) and in Switzerland and can also depend on whether you receive a UK State Pension or some other UK benefits.
You can use a UK-issued European Health Insurance Card (EHIC) or UK Global Health Insurance Card (GHIC) to access healthcare for temporary stays, usually up to 90 days.
Find out how to apply for healthcare cover abroad (GHIC and EHIC)
Once you’re registered to live and work in an EU country or Switzerland, you should not use your EHIC or GHIC to get healthcare in that country. However, you may be able to get an EHIC card from that country for travel. If you live in an EU country or Switzerland, you may also be eligible to apply for an S1 form for entitlement to state healthcare paid for by the UK once you begin to draw a UK State Pension.
You will not be covered for healthcare paid for by the UK if you’re going to live permanently outside the EU and Switzerland.
Posted workers
If you’re a worker temporarily posted by a UK company to an EU country, Norway, Iceland, Liechtenstein or Switzerland, you may be entitled to health cover funded by the UK in the country you’re posted to.
You can find out your National Insurance status from HM Revenue and Customs (HMRC):
Contact HMRC about your National Insurance and health cover abroad (UK residents) on GOV.UK
Contact HMRC about your National Insurance and health cover abroad (non-UK residents) on GOV.UK
If you move to an EU country or Switzerland and you receive a UK State Pension, you may be entitled to state healthcare paid for by the UK.
You’ll need to apply for a certificate of entitlement known as an S1 form. S1 forms show that your state healthcare is paid for by the UK if you live in an EU country or Switzerland.
If you’re applying for an S1 form in Switzerland, you’ll need to satisfy additional nationality criteria to be eligible. You’ll only be issued with an S1 in Switzerland if you’re a UK national, a Swiss national, an EU citizen, a refugee or a stateless person, or if you’re the family member or survivor of someone who has one of these nationalities or statuses.
If you receive both a pension from the country you now live in and your UK State Pension, you cannot get an S1 form. This is because the country you live in will be responsible for your healthcare. If you receive your UK State Pension as well as a pension from an EU member state, but are now living in a different EU state, the country to which you paid contributions toward your pension for the longest period becomes responsible for your healthcare.
Healthcare if you have an exportable benefit
If you’ve been living in an EU country, Norway, Iceland, Liechtenstein or Switzerland since before 1 January 2021, and you receive contribution-based Employment Support Allowance or some other exportable benefits, you may also be entitled to an S1 form.
Read more about claiming benefits if you live, move or travel abroad on GOV.UK
How to get an S1 form
You can apply for an S1 form from the Overseas Healthcare Services.
Telephone: +44 (0)191 218 1999
Email: s1applications@nhsbsa.nhs.uk
Monday to Friday 8am to 6pm (GMT) You can apply for an S1 form up to 90 days before moving to live in an EU country. You can ask for the form to be sent to your UK address if you need it for your visa application.
For the S1 form to be issued, you need to have an address in the EU country you are moving to. This can be a temporary address, but you must contact NHS Business Services Authority (NHSBSA) and the relevant authority in the country you are moving to, to let them know your new address (if it changes). This is to prevent important confidential information being sent to the wrong address.
How to use an S1 form
Once issued, register the S1 form with the relevant authority in your country of residence.
Often you need to do this before you can register for healthcare or obtain a medical card.
If you have registered an S1 in an EU country, you’ll be able to use your UK-issued EHIC or GHIC to access state-funded necessary medical treatment when you visit other EU countries. You’ll not be able to use it in Switzerland.
Changes to who can get an S1 form
The rules have changed around S1 cover for people who claim the following exportable benefits:
- Disability Living Allowance (DLA)
- Personal Independence Payment (PIP)
- Carer’s Allowance (CA)
- Attendance Allowance (AA)
These benefits currently entitle you to an S1 form if you moved to an EU country, Norway, Iceland, Liechtenstein or Switzerland before 1 January 2021, for as long as you receive that benefit.
If you do not yet have an S1 form
You can no longer get an S1 form based on receiving one of the exportable benefits listed above.
However, it may still be possible to receive an S1 if you export your Maternity Allowance or certain qualifying industrial accident or bereavement benefits.
Read more about claiming benefits if you live, move or travel abroad on GOV.UK
You may also be entitled to an S1 form through exporting a UK State Pension or other qualifying benefit if you are in scope of the Withdrawal Agreement.
If you already have an S1 form
You’ll continue to be covered by your S1 form if you already have one for as long as you’re receiving one of the above benefits.
If you have a time-limited S1 form, you can apply to renew it, as long as you’re still receiving one of the benefits listed above.
Further information about accessing NHS services can be found on the visiting or moving to England pages
Privacy Notice
Click here to view our privacy notice

Privacy Notice – Children
Click here for our Privacy Notice for Children
Subject Access Request Form
Subject Access Request
Requesting copies of medical records or extract from medical records.
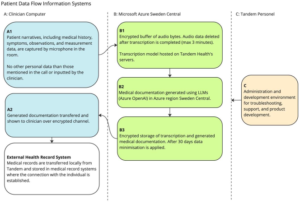
Tandem
Some of our clinicians at Arcadian Gardens Surgery are currently utilising a dictation AI software called Tandem to summarise their consultations when you visit them:
Zero Tolerance Policy
Arcadian Gardens Surgery operates a ‘zero-tolerance’ policy towards aggressive or abusive behaviour. This includes any personal, abusive or threatening comments, bad language, physical contact and aggressive gestures. In keeping with the rest of the National Health Service, this means that no abuse of our staff is acceptable, whether verbal or physical. Any patient behaving in this manner will be removed from the practice list with immediate effect. In some cases, the police will be called.
Introduction
The Practice takes it very seriously if a member of staff is treated in an abusive or violent way.
The Practice supports the government’s ‘Zero Tolerance’ campaign for Health Service Staff. This states that GP practices and their staff have a right to care for others without fear of being attacked or abused. To successfully provide these services a mutual respect between all the staff and patients has to be in place.
The team at Arcadian Gardens Surgery aims to be polite, helpful, and sensitive to all patients’ individual needs and circumstances. We respectfully remind patients that very often staff could be confronted with a multitude of varying and sometimes difficult tasks and situations, all at the same time. We understand that ill patients do not always act in a reasonable manner and will take this into consideration when trying to deal with a misunderstanding or complaint.
However, aggressive behaviour, be it violent or abusive, will not be tolerated and may result in you being removed from the Practice list and, in extreme cases, the police being contacted.
In order for the practice to maintain good relations with our patients, we would like to ask them all to read and take note of the occasional types of behaviour that would be found unacceptable:
- Using bad language or swearing at practice staff
- Any physical violence towards any member of the Primary Health Care Team or other patients, such as pushing or shoving
- Verbal abuse towards the staff in any form including verbally insulting the staff
- Racial abuse and sexual harassment will not be tolerated within this practice
- Persistent or unrealistic demands that cause stress to staff will not be accepted. Requests will be met wherever possible and explanations given when they cannot
- Causing damage/stealing from the Practice’s premises, staff or patients
- Obtaining drugs and/or medical services fraudulently
We ask you to treat your GPs and their staff courteously at all times.
The Legal Position
As a responsible employer, the Practice has a duty as a provider of NHS healthcare to protect the health, safety and welfare of staff under the Health & Safety at Work Act. This includes a risk assessment of violence towards staff and taking steps to mitigate this under the Management of Health and Safety at Work Regulations 1999.
Staff members who are victims of violent conduct or assault have the right to sue their employers for compensation if the risk of violence could have been reduced or removed completely, but the employers did not act upon this information.
Examples of security issues:
- Security of grounds and car parking
- Security of premises – incl. storage, “out of hours”
- CCTV
- Cash and staff – storing, handling and transferring
- Security Systems
- Security of equipment – medical devices, computers
- Communication of national security alerts
- Information records
- Contingency planning.
- Security of employees
- Staff working on their own
- (Staff can be lone workers when making domiciliary visits or within a hospital department e.g. out of hours)
This list is not exhaustive.
For example, a lone working risk assessment must provide the lone worker full knowledge of the hazards and risks to which he or she is being exposed and what they must need to do will something go wrong. Other responsible persons must know the whereabouts of lone workers and what they are doing.
Violence At Work
The practice acknowledges that there may be instances where violence and / or aggression forms part of a patient’s illness. In these circumstances, the issue will be discussed with the patient and form part of their care planning.
This information will be recorded in the patient’s medical record and flagged to ensure that members of staff are aware. In addition, where deemed necessary, appropriate support will be put in place, e.g. staff members do not see the patient alone.
Definition Of Physical And Verbal Abuse And Violence
Physical and verbal abuse includes:
- Unreasonable and / or offensive remarks or behaviour / rude gestures / innuendoes
- Sexual and racial harassment
- Threatening behaviour (with or without a weapon)
- Actual physical assault (whether or not it results in actual injury) includes being pushed or shoved as well as being hit, punched or attacked with a weapon, or being intentionally struck with bodily fluids or excrement.
- Attacks on members of staff or the public
- Discrimination of any kind
- Damage to an employee’s or employer’s property
Zero Tolerance Stance Adopted By The NHS
The Practice supports the Zero Tolerance stance adopted by the NHS.
The HSE (Health and Safety Executive) defines work-related violence as:
“Any incident, in which a person is abused, threatened or assaulted in circumstances relating to their work”.
Violence and aggression towards a person may also be defined as:
“A physical contact with another person which may or may not result in pain or injury. The contact is uninvited and is an attempt to cause harm, injury or to intimidate. Non-physical aggression includes the use of language which causes offence or threatens the safety of a member of staff”.
The Health And Safety at Work Act 1974
Under the Health and Safety at Work Act 1974, the practice will also undertake the following measures to ensure a safe work environment:
- Carry our risk assessments to assess and review the duties of employees, identifying any “at risk” situations and taking appropriate steps to reduce or remove the risk to employees, particularly if they are working alone.
- Assess and review the layout of the premises to reduce the risk to employees where physically possible.
- Assess and review the provision of personal safety equipment, such as alarms.
- Develop surgery policies, procedures and guidelines for dealing with physical and verbal abuse.
- Provide support and counselling for victims, or refer to suitably qualified health professionals.
- Make employees aware of risks and ensure employee involvement in suitable training courses.
- Record any incidents on a Significant Event form and take any remedial action to ensure similar incidents are prevented in future.
Removal From The Practice List
The removal of patients from our list is an exceptional and rare event and is a last resort in an impaired patient-practice relationship. We value and respect good patient-doctor relationships based on mutual respect and trust. When trust has irretrievably broken down, the practice will consider all factors before removing a patient from their list, and communicate to them that it is in the patient’s best interest that they should find a new practice. An exception to this is in the case of immediate removal on the grounds of violence e.g. when the Police are involved.
Removing Other Members Of The Household
Because of the possible need to visit patients at home, it may be necessary to terminate responsibility for other members of the family or the entire household to ensure the safety of practice staff.
The prospect of visiting patients that is the residence of a relative who is no longer a patient of the practice, or the risk of being regularly confronted by the removed patient, may make it difficult for the practice to continue to look after the whole family. This is more likely where the removed patient has been violent or displayed threatening behaviour, and keeping the other family members could put doctors or their staff at risk.
An exception to this is in the case of immediate removal on the grounds of violence (e.g., when the Police are involved), or in cases of sexual harassment. Any form of sexual harassment, whether verbal, physical, or otherwise, will result in the immediate removal of the patient from our list, as this behaviour is unacceptable and breaches the fundamental principles of respect and trust in the patient-practice relationship.